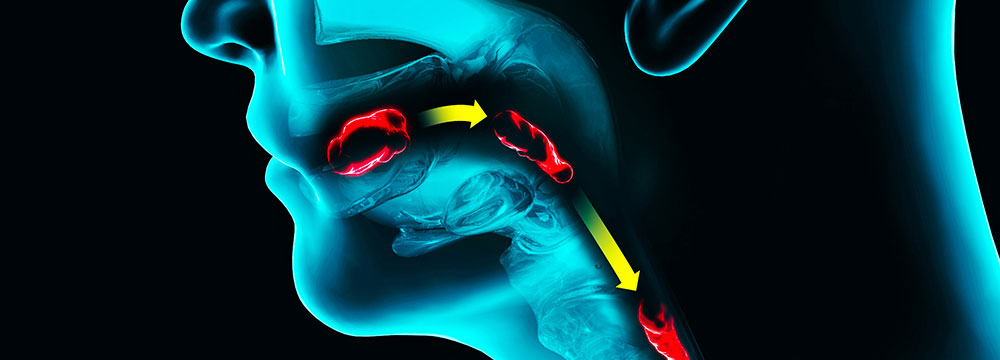
Swallowing gone wrong in EoE
Eosinophilic esophagitis (EoE) is uncommon but also underdiagnosed: Patients may not seek care for their symptoms, and physicians may not be aware of the condition.
Swallowing is like breathing: It happens all the time, and yet, “You don't notice anything about it unless it goes wrong,” said gastroenterologist Evan S. Dellon, MD, MPH.
Eosinophilic esophagitis (EoE) is one condition where swallowing goes wrong. Symptoms of the chronic, immune-mediated disease include esophageal dysfunction, such as dysphagia, vomiting, or feeding difficulties, and eosinophilic infiltration of the esophageal mucosa.
While EoE is uncommon, with an estimated prevalence of about 0.5 to 1 in 1,000 people, it is underdiagnosed, said Dr. Dellon, a professor of medicine and director of the Center for Esophageal Diseases and Swallowing at the University of North Carolina at Chapel Hill School of Medicine. That's because patients don't seek care for their symptoms and because clinicians may be unaware of the condition, he noted.
One consequence of not receiving a diagnosis is food impaction, which can send patients to the ED. The annual volume of EoE-associated ED visits tripled from 2009 to 2019 and is projected to double again by 2030, according to a study published in May by Clinical Gastroenterology and Hepatology.
During the study period, the authors identified 50,000 ED visits with an EoE diagnosis code and found more than 700,000 ED visits for dysphagia, food impaction, or esophageal stricture in men younger than age 40 years without a formal EoE diagnosis. “I think we're seeing the tip of the iceberg, and as there's more education, both on the patient and provider side, we'll probably see more and more diagnosis,” said Dr. Dellon, a coauthor of the study.
Gastroenterologists manage most patients with EoE; however, they rely on primary care physicians (PCPs) to recognize the symptoms and refer patients to gastroenterology for diagnosis via endoscopy. Experts explained what internal medicine physicians need to know about EoE diagnosis and management.
Sussing out symptoms
EoE has a relatively brief history. While the first cases were reported in the late 1970s, the disease was initially characterized in the early 1990s, according to a review published in 2018 by Gastroenterology.
“Since then, EoE has transformed from a rare case-reportable condition to a disease that is commonly encountered in the clinic and endoscopy suite, and a major cause of upper gastrointestinal morbidity and increasing health care costs,” the authors wrote.
Although EoE affects patients of all ages, the average age at diagnosis in adults is the mid-30s, noted gastroenterologist Nirmala Gonsalves, MD. EoE also affects more men than women in about a 3:1 distribution, and prior reports suggest it is more common in White patients. “However, recent data suggest that this condition has been underreported in other races, so it's important for clinicians to know that it can affect any age and race and should be suspected in all patients presenting with difficulty swallowing,” she said.
As for why EoE occurs, the current thinking is that certain genes may predispose patients in addition to exposure to food and environmental allergies, said Dr. Gonsalves, who is a professor of medicine and co-director of the Eosinophilic Gastrointestinal Disorders Program at Northwestern University Feinberg School of Medicine in Chicago.
“Due to those genes ‘turning on,’ so to speak, patients will get reactions in their esophagus when they're exposed to common foods, triggered by certain allergic cell signals that cause the body to react to these foods,” she said. “So we know this is a food allergy-triggered condition, and common foods in our diet can drive this inflammation.”
Those food culprits, ordered from most to least common, are milk, wheat, soy, egg, nuts, and seafood, said Dr. Gonsalves, who was one of the first to research the identification and elimination of food triggers as a way of healing EoE in adults. “Our data at Northwestern suggest that 70% of patients will have just one food trigger, which is great because they don't have multiple things that they have to avoid,” she said.
EoE commonly presents in patients with other allergic disorders, such as atopic dermatitis, allergic rhinitis, asthma, hay fever, and seasonal allergies, Dr. Gonsalves said. “We think the incidence and prevalence is rising, similar to other allergic disorders,” she said. “For instance, clinicians are seeing more cases of asthma and food allergies, which are increasing similarly to what we are seeing with EoE.”
Recognizing symptoms is critical to identifying patients with EoE. Internal medicine physicians may be more accustomed to asking about symptoms of another esophageal disorder, gastroesophageal reflux disease, but symptoms of EoE are more about esophageal transit of food movement through the esophagus than heartburn or regurgitation, Dr. Gonsalves said.
If there is suspicion for EoE, one of the most important symptoms to ask about is dysphagia; however, asking about this one symptom often isn't enough, she said. That's because many patients with EoE self-manage their symptoms through behaviors like avoiding certain foods and textures, lubricating their foods, chewing very well, and eating very slowly, said Dr. Gonsalves.
“If you were to ask a typical EoE patient, ‘Are you having difficulty swallowing?’ the majority of them would say no,” she said. “But doing a little bit of a deeper dive into how they're eating, if anything that they're eating actually feels a little sticky going down or is going down slowly, or if they're having to avoid certain foods … can uncover this diagnosis.” The clinician could also have the patient describe how they would eat something like a dry bagel, Dr. Gonsalves added.
Of course, adding these questions to a visit is a big ask for busy PCPs, said gastroenterologist and ACP Member Joy Chang, MD, MS, an assistant professor of medicine at the University of Michigan in Ann Arbor. “But if PCPs can screen for these concerning symptoms, that would be very impactful,” she said. “Send them to GI, and we can make the diagnosis.”
Since that requires an endoscopy with biopsies, making a referral to gastroenterology is a must when EoE is suspected, Dr. Chang said. Diagnostic criteria of EoE include symptoms of esophageal dysfunction, 15 or more eosinophils per high-power field on esophageal biopsy, and assessment of non-EoE disorders that cause or potentially contribute to esophageal eosinophilia, according to the 2018 international consensus guidelines, which were published in Gastroenterology.
Before making the referral, though, it is helpful to know whether the patient is taking a proton-pump inhibitor (PPI), which can treat EoE symptoms and mask the disease on endoscopy, Dr. Chang advised. “Many times, people referred to me are already on the PPI prior to an endoscopy, and in these cases, it can be challenging to know if they have EoE or not,” she said. “Since PPIs can be an effective treatment for EoE in nearly half of individuals, oftentimes making a clear diagnosis of EoE requires stopping the PPI, then performing the endoscopy with biopsies.”
Effective treatments
In addition to PPIs, several treatment options are available for patients with EoE, although they are generally prescribed by a gastroenterologist rather than a PCP, the experts said. These include swallowed corticosteroids (e.g., a fluticasone inhaler and oral viscous budesonide) and dietary therapy, although they are not FDA approved to treat EoE, according to a 2021 JAMA review.
Compared with a response rate of 13.3% in a historical placebo comparison group, research data showed a pooled histologic response to treatment of 41.7% with PPIs, 64.9% with swallowed topical corticosteroids, 93.6% with an elemental diet exclusively made up of amino acid-based formula, and 67.9% with a six-food elimination diet that nixes milk, wheat, soy, egg, nuts, and seafood, according to the review.
Each of these treatments is better than no treatment, according to 2020 guidelines from the American Gastroenterological Association and the Joint Task Force (AGA/JTF) on Allergy-Immunology Practice Parameters. Compared with no treatment, the AGA/JTF suggests using PPIs (very low-quality evidence), strongly recommends topical corticosteroids (moderate evidence), suggests using an elemental diet (moderate evidence), and suggests using an empiric six-food elimination diet (low-quality evidence).
With a lack of comparative studies, treatment should be individualized to the patient based on their preferences using shared decision-making, said Dr. Dellon. “Do you want to try the diet elimination and try to figure out what the food triggers are, or do you want to try a medicine? For me, that's a big differentiating point,” he said.
Even though data show that dietary therapy is as effective as medications for EoE, gastroenterologists rated it as the least effective treatment in a survey study published in the December 2022 American Journal of Gastroenterology. The greatest barrier they cited was the perception that patients were not interested in or were unlikely to accept or adhere to the diet.
Those who select dietary therapy typically want to address “what a lot of patients call the root cause, which actual food trigger is causing this whole thing to happen, and eliminating that,” said Dr. Chang, who was lead author of the study. Dietary therapy is a great option for many patients, especially when they're motivated to make dietary changes and prefer to treat their EoE with a nonpharmacologic strategy, she said.
“Since removing specific food groups can be challenging, partnering with a dietitian is important in the success of the elimination diet, identifying the specific EoE food triggers, and adherence to this therapy,” Dr. Chang noted. “Downsides of dietary therapy include temporary dietary restrictions and multiple endoscopies required to identify the food trigger or triggers, but for many patients, this is a desired and effective way to manage EoE.”
Monoclonal antibodies are another potential therapeutic option and are being evaluated in clinical trials. In 2022, dupilumab became the first FDA-approved treatment for EoE, which was “a huge milestone in the field,” said Dr. Dellon, who has researched the drug for Sanofi and Regeneron Pharmaceuticals and has served as a consultant for and received research funding from both companies. The weekly subcutaneous injection is indicated to treat EoE in patients ages 12 years and older weighing at least 40 kg.
“To have it for severe patients is really terrific. We were all really excited when that [approval] happened,” said Dr. Dellon. “It's a little bittersweet, though, because for a lot of the people who are diagnosed right off the bat or who may be a little bit more mild, we still don't have anything approved, so it kind of highlights that gap in our treatment options right now.”
At this point, dupilumab is very expensive, he noted. “For insurance purposes, you usually have to demonstrate that you don't respond to other treatments first, so I'm still using the PPIs or steroids as first-line treatments,” Dr. Dellon said.
Patients should continue treatment for the long run, Dr. Chang noted, and EoE guidelines recommend maintenance therapy to prevent disease recurrence. “This disease quickly recurs once you stop the therapy that's keeping EoE in remission … so we do advocate for people to stay on their treatments,” she said.
Gastroenterologists usually monitor patients with EoE on a regular basis; however, the disease doesn't necessarily call for endoscopic surveillance for cancer, unlike Barrett's esophagus, Dr. Chang said. “Management of Barrett's esophagus requires surveillance endoscopy at least every three to five years because of the small but nonzero risk of progressing to a cancer. A precancerous risk has not been identified for EoE to date,” she said. “So whether or not to relook every couple of years is more variable, depending on the patient's disease and provider practice.”
Even though there's no increased cancer risk, there are serious consequences to untreated EoE, Dr. Dellon noted. “The longer you have symptoms before diagnosis, the higher the chance that you'll have strictures in the esophagus that need dilation,” he said. “And food impactions, it's not a minor thing; you could have esophagus injury or rupture.”
About 1% or 2% of the EoE population has had a perforation in the esophagus, most commonly from a food impaction but sometimes from the endoscopy treating the impaction, Dr. Dellon noted. “That's really the riskier time for those patients, so it can make a huge impact to treat them.”
Ultimately, the internal medicine physician's role in EoE is to recognize the symptoms, have a high index of suspicion, and refer patients with suspected EoE to gastroenterology for diagnosis, experts said. Once an EoE diagnosis is confirmed, it can be life-changing for patients.
“People are afraid of their business lunches or in public settings to eat because they're worried that they're going to have an embarrassing episode where the food gets stuck or they bring it back up at the table, so it's very, very impactful to make the diagnosis and institute treatment,” Dr. Dellon said.
Patients also express relief and feel validated when they're finally diagnosed, Dr. Gonsalves said. “They're telling us, ‘Oh, I've been swallowing like this my whole life, and I just thought it was just me. I never knew swallowing could be normal,’ once we get them on treatment and open up that esophagus,” she said.




