‘Discontinued’ medications a problem when using EHRs
Physicians who wonder why a patient is still taking a discontinued medication might look to their EHRs for the answer. Unlike with new prescriptions, a doctor's orders to stop a drug usually aren't automatically transmitted to pharmacies. This widespread problem requires an old-fashioned solution: talking to patients to ensure they know what medications they are meant to be taking.
Physicians who wonder why a patient is still taking a medication discontinued months ago might turn to their electronic health record (EHR) for the answer. Most EHRs can automatically transmit new prescriptions to pharmacies, but orders to stop a medication still need to be processed manually.
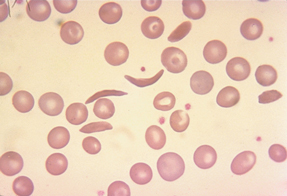
A retrospective cohort study published in the Nov. 20, 2012, Annals of Internal Medicine examined this problem in one multispecialty group practice in eastern Massachusetts, looking specifically at long-term medications that could cause harm when used inappropriately: antihypertensive agents, antiplatelets, anticoagulants, oral hypoglycemic agents and statins. The study found that of 83,902 electronically discontinued medications, 1,218, or 1.5%, were dispensed by a pharmacy at least once during the next 12 months.

Adrienne S. Allen, MD, MPH, the study's lead author and a physician at North Shore Physicians Group in Danvers, Mass., recently spoke to ACP Internist about her study's findings and some possible solutions.
Q: What's causing this problem? Are physicians assuming that when they discontinue a medication in the EHR, the information is going right to the pharmacy?
A: Yes. If you had a paper prescription, you would never assume that any type of information would go to the pharmacy. But with electronic prescribing, you sit at a computer and send [the information] over. With most electronic health records, when you stop the medication, they often ask you why.
[The EHR] appears to do something with that information. It gives the impression that the information's going somewhere when in fact it's not. With e-mails, things go both ways, so you might assume that the medications do, too.
Q: In your study, medications that were discontinued still ended up being dispensed 1.5% of the time, correct?
A: Exactly. My study was limited in that it was only looking at internal pharmacies. We were in a closed group model, so about 50% of prescriptions are internal and 50% are external. Our study only looked at our internal pharmacies, but if it's that type of rate for our internal pharmacies, we'd imagine it would be the same rate or even higher for a [commercial pharmacy] for the same process.
Q: Was 1.5% about the rate you expected?
A: I didn't know what to expect. The reason I did the study is it happened to me. I started to look into it after a patient whose medication I had discontinued came back in on it. When I discontinued the medication from the record, I assumed that the pharmacy would have known about it.
As I started investigating, there was really nothing in the literature about this and no one seems to know that this happens. Pharmacists are aware that this is the case, but clinicians aren't aware that this is a really common thing. It seems like a small number, but if you multiply that over the amount of prescriptions we do throughout the year, it's a concerning number.
Q: Your study took place in one health system, but do you think this is a widespread problem, given increasing EHR use?
A: Yes. The Veterans Administration is the only place I know where if a medication is discontinued, the pharmacy is aware of it. It is a widespread problem.
Q: In your study, how many cases of potential harm did you find?
A: We did a selective chart review, and if we extrapolate, about 12% of medications that were dispensed erroneously had harm [associated with them]. Most frequently, patients had a clinical reaction, such as low blood pressure, slow heart rate, cough and lightheadedness. Laboratory abnormalities were the second most common [adverse effect], like hyponatremia and elevated liver function tests.
Q: So most of the events were problems that weren't immediately life-threatening but could cause damage over time?
A: Exactly, or doctors would be trying to figure out “Why does my patient have a cough?” and later find out “They're still taking that lisinopril I discontinued a few months ago.”
Q: Do automatic refills play a role in this problem?
A: That's a whole other area that we didn't look at. But it's another area that can cause confusion in the medication list. Research could explore whether a master med list should live somewhere.
Pharmacies send reminders to the patient—”You have refills ready”—and to the doctor's office—”This patient is out of X medication. Please automatically refill.” Both types of reminders can cause confusion in the office. Who owns that master med list? A lot of work needs to be done about where that list should live.
Q: If patients went to the pharmacy and had an automatic refill waiting for them, might they think a discontinued medication had been restarted?
A: Yes. In our study, patients who were on 15 or more medications were more likely to have a medication dispensed when there was no active order. The more you are on, the more likely that confusion is going to happen. It's about education when the patient's in the office, not only “Here's your active med list and please check,” but “If it's not matching exactly when you go to the pharmacy, please call back.”
Q: What are some short- and long-term potential solutions?
A: Over the short term, [we need] more patient communication. Until a fix can happen, it's so important for patients to know what they're taking, and I think often they aren't sure. At the end of the visit, patients need to get a printed list of their updated medications. At the pharmacy, they should check the names of the pills that they're getting and the dosage, that they exactly match what's on that list, that if there are any discrepancies to call their doctor. In the meantime, we hope to have people explore fixes, but this is what patients can do here and now.
For a long-term fix, we should be able to send a discontinuation notice, ideally back to the same pharmacy that received the initial order. Internally, at the place where my study was done, they are working on that fix. The technology exists, but there are logistics that would need to be worked out, for example, what happens when patients use multiple pharmacies.
It's a matter of getting a partner, maybe one of the large EHRs, to work with us, to look at a systematic fix. It's a matter of having people willing to receive [the information], and working out what that workflow would look like.