Business experts urge small-practice doctors to take action
Speakers at a recent Business of Medicine Summit had some grim predictions and urgent alerts for attendees: “Start preparing for that storm that's partly on the coast but not here yet.”.
At the Business of Medicine Summit held in Philadelphia this February, speakers had some grim predictions and urgent alerts for attendees.
“Start preparing for that storm that's partly on the coast but not here yet,” said Michael Barr, MD, MBA, FACP, senior vice president of medical practice, professionalism and quality for ACP, which co-sponsored the medical education event with the Institute for Continuing Healthcare Education and the Jefferson School of Population Health.

The approaching tumult for physicians includes the conversion to ICD-10, migration from fee-for-service to outcome-based payment, and tax law changes, according to the experts present.
ICD-10
Many physicians are assuming that the warnings about ICD-10 are overblown, according to Jay Sultan, a consultant and associate vice president of The TriZetto Group in Athens, Ga. In a recent survey of 801 medical practices by Gateway EDI, more than three-quarters had not started implementation for the planned October 2014 switch.
“Physicians largely believe that they are not going to have to do ICD-10. A lot of them are saying, ‘Hey maybe it will be ICD-11. I'll just wait,’” said Mr. Sultan.
The laggards may have grounds for believing that implementation will be delayed again (although likely not as far as 2016, when ICD-11 is scheduled to appear), but that doesn't mean they shouldn't be getting ready. “If you think that ICD-10 is no longer something to worry about, you're wrong,” he said. “You are facing your practice going out of business if you are not preparing to be ready for ICD-10.”
The switch is likely to pose problems from a number of directions. “The biggest [potential] costs are lost or delayed revenue because suddenly your claims stop getting paid,” said Mr. Sultan. Practices should plan for the possibility that payments from commercial payers could be delayed by technical snafus for as long as six months. Payers have been slow to prepare for the transition, too, he noted.
“Find out what your payers are going to do. Are your payers going to be willing to go ahead and write you an advance check while the claims are being cleaned up?” Mr. Sultan said. Establishing a line of credit in advance might be another solution to this potential problem.
Even if the transition goes smoothly, payments will change under ICD-10.
“Under the new code, there are things that you used to get paid $100 for, now you get paid $50 for,” said Mr. Sultan. “Review all of your contracts, and understand how the payers' changes in the contracts are going to affect your reimbursement. Focus on your high-volume diagnosis procedure codes.”
He estimated that transitioning to the new system is likely to cost practices anywhere from $84,000 to $2.7 million, depending on size, with costs coming from education and training, decreased productivity and accuracy, and delayed or denied claims.
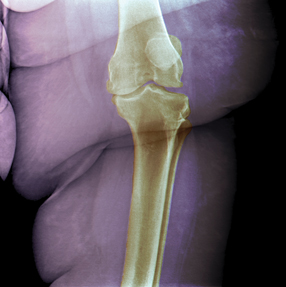
Mr. Sultan also offered two anecdotes about ICD-10, one positive and one negative. On the positive side, medical examiners' implementation of ICD-10 in 1999 revealed the vast number of patients who die as a result of a fall on a level surface.
“Through the better coding they figured that out, and now there are lots of different programs working on trying to reduce that statistic,” he said. “My point is ICD-10 is actually kind of useful, as much as we hate to say it.”
The darker news comes from Canada's implementation of ICD-10. “They saw a 50% decrease in productivity in the first six months—20% never regained—and after a couple years, they canceled the whole program,” said Mr. Sultan. “We probably won't have that luxury.” (For more on the conversion to ICD-10, see the Practice Rx column on page 8 of this issue.)
Risk-based payments
Another luxury physicians can't afford is ignoring the trend toward payment based on patient outcomes, according to Mr. Sultan. “In 10 years, you will no longer be able to be successful if you let somebody else do your contracting off in a vacuum,” he said. “Everybody is going to be faced with the burden of taking on risk-based contracts.”
Before agreeing to a payment deal that hinges reimbursement on patients' results, physicians need to assess how they can actually affect those results, Mr. Sultan emphasized. “I cannot tell you how many providers do this backwards,” he said. “Make sure that whoever writes your contracts has started with the analysis, instead of starting with the price. These new payment methods are not magic pixie dust.”
To succeed in a risk-based payment model, a physician has to find ways to reduce costs and improve outcomes. “Target your highest-risk patients and figure out what it will take to lower their costs,” said Mr. Sultan.
The answer will likely be a combination of changes by your practice, the patients and other clinicians. For example, one solution might be having a nurse routinely call high-risk patients to identify problems early enough to avert hospitalization. Patients' behavior can be changed with incentives and amenities, said Mr. Sultan, citing a practice that bought a taxi company to reduce no-shows and a hospital that gave gift cards to patients who attended education sessions.
Finding all the excess costs involved in a patient's care will require significant data gathering. “If you're suddenly responsible for the cost of this patient, you've got to know which are the $600 colonoscopy sites and which are the $6,000 colonoscopy sites,” Mr. Sultan said.
Unfortunately, most electronic medical records do not provide the necessary information, he said. “You have to ask yourself if in addition to all those mind-numbing things you have to do with your EMR [to attain meaningful use], are you making your patients better?” he said. “Does your system tell you what guidelines you're missing? Does it tell you your patient went to the ‘doc in a box’ four times last month?”
Gathering and acting on these data are complex enough that many practices will need to hire a risk manager. The good news, Mr. Sultan said, is that many of them are available for hire, as insurers have less need for them under the new payment methods. “These methods put it to a doctor instead of an insurance company to say, ‘What can I do for this patient to make the best possible outcome?’” he said. “Increasingly we're going to see insurance companies playing roles other than being the ultimate arbiter of risk.”
With more than 2,000 risk-based payment programs already under way around the country, this future is coming fast, and independent physician practices might want to hurry to take the lead. “If you want the hospital managing [your payments], then don't do anything. If you want to be in a position where you manage the risk and choose the hospital and vendors, then you're going to have to be in the lead position of contracting risk,” said Mr. Sultan.
Taxes
Change for physicians is not on its way but is already here in the tax system, according to David Mandell, JD, MBA, an attorney with The Law Offices of David B. Mandell, PC, and a financial consultant with The OJM Group, headquartered in Cincinnati.
The Taxpayer Relief Act of 2012, signed by President Obama at the start of 2013, increased the highest tax bracket's rate back up to 39.6%, limited itemized deductions for high-income taxpayers, and increased the capital gains tax. The combination of these changes could add up to a significant increase in tax liability for physicians with higher incomes, according to Mr. Mandell.
“They're paying a higher tax rate but also on more income,” he said. “Tax planning has not been so important since the 1970s.” He recommended that physicians see a forward-looking tax expert, rather than an accountant who simply files tax returns, to develop an individualized response to these changes.
More broadly, though, Mr. Mandell had suggestions about tax-sensitive ways to structure a medical practice. For tax and liability reasons, physicians should never practice under only their own names or in a true partnership, he said: “All your personal assets are liable, and that's also the worst way to operate tax-wise.”
S corporations are the most popular structure for medical practices, and they may allow physicians to take a portion of their income as an owner's distribution, not subject to the Medicare tax (which recently increased to 3.8%), he noted. The C corporation is another popular option, but it does not provide that Medicare tax advantage.
When it comes to retirement planning, however, the C corporation structure offers some extra tax benefits. “The C corporation can sponsor benefit plans that the S corporation can't,” said Mr. Mandell. As a C corporation, for example, a medical practice could sponsor a fringe-benefit plan under section 79 of the tax code.
In a 401(k) or similar retirement plan, you are taxed on your retirement savings at the tax rate in place when you take the money out. Under a Section 79 plan, some of the savings is taxed at today's tax rates, which many experts, including Mr. Mandell, think may prove to be lower than future rates.
“Not many people think they're going back [to the rates of the 2000s],” he said. “With this benefit plan, you can hedge against rates going up. ... and it works well as a supplement to a qualified retirement plan, which most practices already have.”
Determining which type of entity or entities is best for any particular practice (“There's no rule that says a medical practice has to operate as a single entity,” said Mr. Mandell) is not always simple, but it may be tax advantageous, and worth the effort for physicians concerned about their finances.
“You can't be lazy about this,” Mr. Mandell said.