Expert lays out controversies for cardio care
February is National Heart Disease Awareness Month, and the field is wide open to controversies seemingly without resolution when it comes to invasive versus therapeutic regimens.
February is National Heart Disease Awareness Month, and the field is wide open to controversies seemingly without resolution when it comes to invasive versus therapeutic regimens. Evidence-based medicine pits treatments against each other continually, and the trials in support of each modality are legion.
Bill Kussmaul, FACP, an associate editor of Annals of Internal Medicine, addressed some of the hottest controversies in cardiology. His tips and insights are invaluable to busy primary care physicians looking for the bottom line on thorny issues. Dr. Kussmaul is the associate director of the cardiac catheterization laboratory at Hahnemann University Hospital in Philadelphia. A podcast of this edited transcript is available at Better Health.
Cholesterol and statin therapy
Q: Who should receive high-dose statin therapy?
A: Cholesterol measurement and treatment guidelines have been evolving over time. At one point clinicians only looked at their patients' total cholesterol, but now we know that there is “good” (HDL) and “bad” (LDL) cholesterol. The recent controversy has been about how low we should go with LDL targets. Should our goal be 130, 100, or 70 mg/Ll? Also, there's controversy about whether or not LDL targets matter that much, or if higher doses of statins, regardless of blood levels of LDL, are simply better for patients.
Q: And what about the high-sensitivity CRP test? Should that be used as a screening tool?
A: My highly educated patients ask me to check their CRP levels more often than I think is necessary. Enthusiasm about CRP was ignited by JUPITER, where they found that people with low LDL levels but high CRPs benefited from starting statins as a primary prevention strategy.
Q: After JUPITER was released, I remember the media reporting that we may as well put statins in our water supply.
A: Well, we have fluoride in our water, vitamin D in our milk, folic acid in our bread … so we just have to figure out which foodstuff we should put statins in and we'll be all set. I'm being half facetious, but statins are pretty amazing drugs because they seem to have benefits that go beyond what we can measure with cholesterol levels.
Q: So what's your bottom line here with LDL and statin treatment?
A: I think it's best for physicians to follow the NCEP [National Cholesterol Education Program] guidelines . We begin by calculating a patient's Framingham risk (using the standard cardiac disease risk factors that we know and love) to stratify our patients into low-, medium-, and high-risk categories. If a patient has no cardiac risk factors, their LDL target is less than 160 mg/dL. If they're in the high-risk category, they should keep their LDL below 100 mg/dL, and consider trying to get it below 70 mg/dL.
Coronary artery calcium scoring
Q: What is the role of coronary artery calcium scoring? How do you establish if someone is a good candidate for this test, and what do you do with the results?
A: This is one of the hottest controversies in cardiology. The test is non-invasive and can be performed without any contrast. If a study shows that you have no calcium in your coronary arteries, you are very, very unlikely to have a coronary event, whether you're symptomatic or asymptomatic. This makes the test very attractive for ruling out coronary disease.
The problem is that if you do have a little bit of calcium in your arteries, you set the testing train in motion (a stress test perhaps followed by a coronary catheterization, etc.) and you may end up doing more harm than good by screening a lot of asymptomatic patients. The USPSTF [U.S. Preventive Services Task Force] doesn't think there's enough data to support coronary artery calcium scoring for asymptomatic individuals.
However, I think coronary artery calcium scoring would be a great test for the emergency department because patients with chest pain could be sent through the CT scanner and sent home immediately if there was no calcium on the scan. We wouldn't have to check cardiac enzymes and hold them in the ER for at least eight hours.
The other advantage of using a chest CT in the emergency room setting is that you can rule out other urgent concerns with the same test: aortic dissection and pulmonary embolism could be caught while checking for coronary artery calcium, if you are willing to give the patient intravenous contrast.
Coronary CT angiography versus coronary catheterization
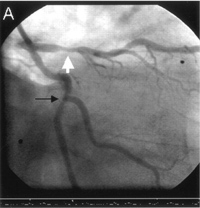
Q: Has coronary CT angiography made coronary catheterization obsolete?
A: The resolution of CT angiography is steadily improving, but remember that CT angiography still subjects the patient to the same amount of radiation as a coronary catheterization, and we're giving them as much dye or more than they'd get with a cath.
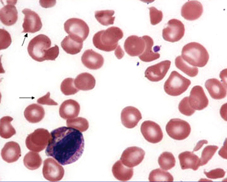
CT angiographies are really good if they're totally normal, but they're not so good if there's plaque in the wall of the arteries. Plaque often contains calcium, and that degrades the CT image. When there's a stent in the artery already, and you're looking for restenosis, the metal from the stent totally degrades the image and you don't get good pictures.
Now, I am an invasive cardiologist so I may have a slant on this, but honestly, I've probably seen more people come to the cath lab because their CT angiography was equivocal than almost any other reason.
To stent or not to stent?
Q: Did the COURAGE trial kill stenting?
A: It started to. But we need to keep in mind that the patients in the COURAGE trial were either asymptomatic or had very stable angina. There is no question that patients admitted to the hospital with unstable angina or acute myocardial infarctions benefit from stenting. The COURAGE trial showed that stable and asymptomatic patients should be managed medically, and only taken to the cath lab if they have symptoms. This isn't really a big revelation. It's appropriate to try conservative measures with patients first, and optimizing their medications is a great place to start.
Q: So does controversy remain about which kind of stents to use?
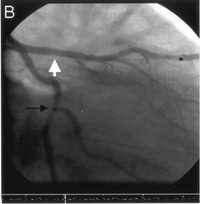
A: Yes, the pendulum has swung pretty hard on this issue. … Drug-eluting stents took the field by storm in 2003, promising the prevention of restenosis. But with most therapies touted as a miracle cure, we find out later that there are some downsides. Unfortunately, while the stents do, in fact, prevent restenosis, we've discovered that stenosis is not what causes heart attacks and deaths. There's also a slightly higher risk of sudden, life-threatening clotting in drug-eluting stents than in bare-metal stents, though the real problem with drug-eluting stents is that they require long-term treatment with anti-platelet agents (like aspirin and clopidogrel) and those are expensive.
That being said, if I needed a stent, I'd choose a drug-eluting stent.