MKSAP Quiz: 3-week history of discharge
A 63-year-old woman is evaluated for a 3-week history of vaginal discharge. The discharge is described as yellowish and malodorous and is accompanied by burning and dyspareunia. She is postmenopausal and is sexually active with a new male partner. Her last Pap smear was 2 years ago and was normal. Medical history is significant for hypertension, and her only medication is hydrochlorothiazide.
On physical examination, the patient is afebrile, blood pressure is 128/78 mm Hg, pulse rate is 72/min, and respiration rate is 12/min. BMI is 26. On pelvic examination, a frothy, yellowish discharge is present in the vaginal vault. The cervix is without lesions, although there is contact bleeding with speculum placement. There is no cervical motion tenderness or adnexal tenderness. The remainder of the examination is unremarkable.
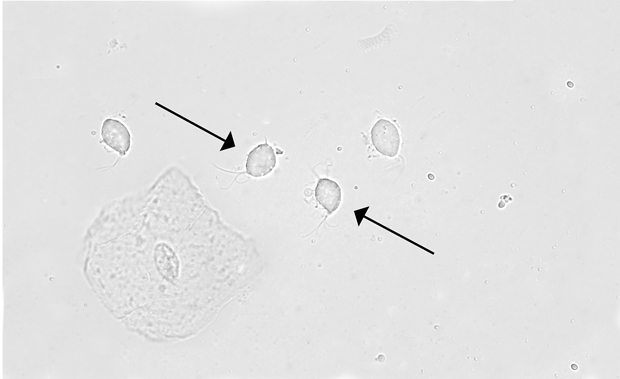
Laboratory studies show vaginal pH is 6.0; whiff test is negative. Saline microscopy is shown. Potassium hydroxide microscopy is negative. Testing for Chlamydia trachomatis and Neisseria gonorrhoeae is negative.
Treatment with single-dose metronidazole is planned.
Which of the following is the most appropriate additional intervention?
A. Confirm infection with a nucleic acid amplification test
B. Perform repeat Pap smear following treatment
C. Test for cure following treatment
D. Treat the patient's sexual partner
Answer and critique
The correct answer is D: Treat the patient's sexual partner. This question can be found in MKSAP 17 in the General Internal Medicine section, item 69.
The most appropriate additional intervention in this patient is to treat her partner. This patient has the characteristic features of frothy yellow discharge, burning, and dyspareunia associated with infection by Trichomonas vaginalis organisms, which are seen on microscopy. Trichomoniasis is the most common curable sexually transmitted infection (STI) worldwide and is evenly distributed among women of all age groups, unlike other STIs that predominate in younger people. It is caused by motile flagellated protozoa that infect the urogenital tract, causing inflammatory vaginitis and urethritis. Treatment with a single 2-g dose of metronidazole is associated with a high rate of cure and should be offered to all symptomatic women. It is important that sexual partners also be treated, even if asymptomatic, because of a high rate of reinfection; documentation of infection is not required before treatment in any partners. Once trichomoniasis is identified, testing for other STIs should be considered in both individuals.
Trichomoniasis has been traditionally associated with a vaginal pH of greater than 4.5 and diagnosed by direct visualization of trichomonads on saline microscopy. However, the specificity of a high vaginal pH and the sensitivity of saline microscopy findings are low. Therefore, point-of-care vaginal swab rapid immunoassays and nucleic acid amplification tests (NAATs) for detection of T. vaginalis are increasingly considered to be the gold standard for diagnosis, and particularly when microscopy is not available. NAATs can be performed on a vaginal (or endocervical) swab, urine sample, or liquid-based Pap test specimens. In this patient in whom trichomonads are seen on microscopy, confirmatory testing with another assay is not necessary.
Trichomoniasis causes an inflammatory vaginitis, and cervical contact bleeding may occur due to inflammation from the infection. This inflammation resolves with treatment of the infection, and a follow-up Pap smear to detect cervical pathology would not be required in the absence of additional symptoms or findings.
Treatment of trichomoniasis with single-dose metronidazole is highly effective; therefore, testing for cure is not required in patients whose symptoms have resolved with therapy.
Key Point
- Trichomoniasis is characterized by copious, malodorous, pale yellow or gray frothy discharge with vulvar itching, burning, and postcoital bleeding; it is effectively treated with a single dose of metronidazole.




