When patients don't tell all: The diagnostic challenge
Patients don't always disclose aspects of their history that may be shameful or stigmatizing, posing a challenge of attribution errors for physicians.
Raghav Govindarajan, ACP Associate Member, a neurology resident at the Cleveland Clinic Florida, told us about a case he saw in India that has important lessons for clinicians everywhere. The patient was a 65-year-old man who presented with chronic symptoms of burning discomfort and weakness in his left leg.
His symptoms had started about seven years prior and he had been told that he had “neuritis.” He reported that he had been treated in the past with corticosteroids, intravenous immunoglobulin and multivitamins without relief of his symptoms. He had seen numerous physicians and was now seeking yet another opinion from a prominent neurologist on the faculty of the hospital in Bangalore where Dr. Govindarajan was a medical student.
“I recall that he was the first patient we evaluated in the afternoon clinic,” he told us. “We often saw 50 patients in a day. The people who came to our hospital were generally very poor and had no insurance. But from the way this man dressed and spoke, we could tell that he came from an affluent background.”
The patient worked as a chief contractor for construction of buildings in the city. He was married and was accompanied by his wife.
The physical exam
Physical examination showed sensory loss as well as motor weakness. There was impaired dorsiflexion and plantar flexion of his left foot. His physical examination was otherwise unremarkable.
Laboratory studies showed a small increase in the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level. There was also a low-titer positive antinuclear antibody (ANA). “Nerve conduction studies were consistent with either an axonal neuropathy or a demyelinating process,” Dr. Govindarajan told us.
“Our leading diagnosis was vasculitis, possibly autoimmune given the elevation in ESR, CRP, and ANA,” Dr. Govindarajan said. “But prior to treatment with corticosteroids, we felt it was important to be certain of the diagnosis, so we recommended a nerve biopsy.”
A return visit
Dr. Govindarajan called the patient at home and asked him to return to the clinic to discuss the rationale for the nerve biopsy and then, if he agreed, sign an informed consent document.
“This time the patient came without his wife,” Dr. Govindarajan said. As the man was presented with the informed consent document, he asked, “Do you think this could be leprosy? One of the doctors I saw previously said that leprosy could be the cause of my symptoms.” On further questioning, he disclosed that he had actually been given anti-leprotic medications but had not completed the full course of treatment.
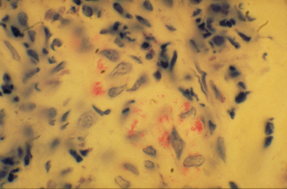
A biopsy of the superficial peroneal nerve on the affected leg revealed bacilli, confirming the diagnosis of peripheral neuropathy due to leprosy. The patient completed a full course of treatment with marked improvement in his symptoms.
Attribution error explained

“I submitted this case because I was reading about cases of leprosy in the United States, and I was reminded of this gentleman,” Dr. Govindarajan said. Indeed, there are approximately 100 cases of the disease reported in the United States each year. Most occur among immigrants. However, cases of leprosy have occurred among Americans who reside in the Southwest due to contact with armadillos, which are hosts for Mycobacterium leprae bacilli.
Dr. Govindarajan told us that leprosy is the leading cause of peripheral neuropathy in India. It is so common that most patients do not undergo biopsy, but are treated empirically with medications including dapsone and rifampin. However, many patients have side effects and stop the drugs before completing a full course.
“I realized that we had made an attribution error in this case,” Dr. Govindarajan told us. “Because the patient came from a higher socioeconomic group, and leprosy usually occurs among the very poor, we did not even consider that diagnosis.” Further, the small elevations in inflammatory and autoimmune markers may have caused the physicians to anchor on a diagnosis of vasculitis.
Stigma's impact on disease care
“There is a cultural stigma associated with leprosy in Indian society,” Dr. Govindarajan told us. “Many patients are ashamed that they have the infection, and some view it as a divine punishment.” This may have been why the patient only disclosed his prior therapy for leprosy when he was alone, unaccompanied by his wife.
The mode of transmission of leprosy is not completely understood, although it is thought that spread may occur through bacilli in nasal secretions. When the route of the transmission of a disease is not well defined, there is fear of even casual contact with affected individuals, reinforcing the stigma of the disease. This was also the case with AIDS before the transmission of HIV was understood.
When patients do not disclose aspects of their history that may be viewed as shameful or stigmatizing, this poses a challenge to all clinicians. We encountered this in the past among patients who ultimately were found to have HIV infection and did not disclose risk factors of sexual contact or drug use. Physicians may be particularly prone to attribution errors with sexually transmitted diseases, not only HIV but also gonorrhea and syphilis, if the patient is assumed to live a lifestyle without risk factors.
As physicians, we should make efforts to foster a sense of trust and confidence that allows patients to comfortably discuss issues that can carry social stigma, but may be important in clinical care.
And whether in the United States or in India, indeed in any part of the globe, we should be mindful of how certain social prejudices may limit the accuracy of the information that we receive from our patients. Further, we as physicians should be aware that our cognitive biases may lead us astray so that we do not ask the right questions to uncover vital information.



